Introduction
In the field of regenerative biotechnology, the limiting factor for tissue repair is often vascularization. Without an adequate blood supply, damaged tissues—particularly hypovascular structures like tendons and ligaments—struggle to access the oxygen, nutrients, and immune cells required for regeneration. This physiological bottleneck has driven significant research into BPC-157 (Body Protection Compound-157), a synthetic pentadecapeptide derived from a protein found in gastric juice.
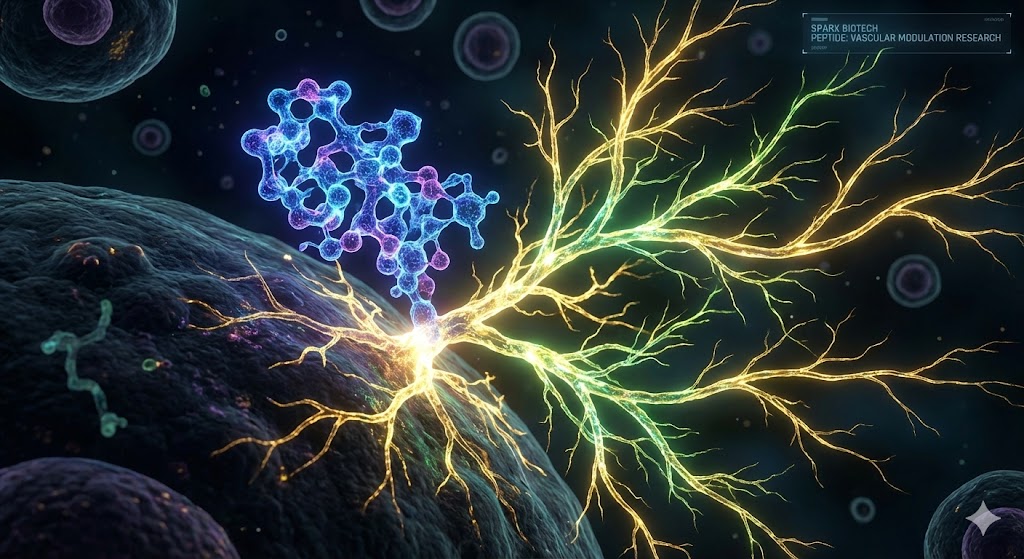
While BPC-157 is widely noted for its cytoprotective properties in the gastrointestinal tract, its potential influence on angiogenesis—the physiological process through which new blood vessels form from pre-existing vessels—has become a central focus of investigation. Current preclinical models suggest that BPC-157 may act as a potent angiomodulatory agent, potentially stimulating the formation of granulation tissue and re-establishing blood flow in ischemic environments.
This article reviews the scientific literature surrounding BPC-157 and angiogenesis, focusing on the proposed molecular mechanisms involving the VEGFR2 pathway, nitric oxide signaling, and vascular remodeling.
The Angiogenic Mechanism: The VEGFR2 Pathway
Angiogenesis is a tightly regulated cascade involving the proliferation, migration, and differentiation of endothelial cells. Central to this process is Vascular Endothelial Growth Factor (VEGF) and its primary receptor, VEGFR2.
Research published in journals such as the Journal of Physiology and Pharmacology and Scientific Reports has elucidated a specific pathway by which BPC-157 may interface with this system. Unlike exogenous growth factors that act directly as ligands, studies indicate that BPC-157 may upregulate the expression and activation of the VEGFR2 receptor itself.
1. VEGFR2 Internalization and Activation
In vitro studies using human umbilical vein endothelial cells (HUVECs) have observed that BPC-157 exposure correlates with increased internalization of VEGFR2. Internalization is a critical step in signal transduction, moving the receptor from the cell surface to intracellular compartments where it initiates downstream signaling.
2. The Akt-eNOS Signaling Axis
Once activated, the VEGFR2 pathway triggers a phosphorylation cascade. Research suggests BPC-157 promotes the phosphorylation of Akt (Protein Kinase B), which subsequently activates eNOS (endothelial nitric oxide synthase). This specific signaling axis (VEGFR2-Akt-eNOS) is a well-established driver of endothelial cell survival and proliferation.
Modulation of the Nitric Oxide (NO) System
The relationship between BPC-157 and the Nitric Oxide (NO) system is one of the most distinct aspects of its research profile. Nitric oxide is a gasotransmitter that governs vasodilation (the widening of blood vessels) and vascular homeostasis.
In standard physiology, NO production must be balanced; too little leads to vasoconstriction and ischemia, while uncontrolled production can lead to oxidative stress.
The "Angiomodulatory" Effect
Scientific literature often describes BPC-157 as "angiomodulatory" rather than strictly "pro-angiogenic." This distinction is vital in research contexts.
- In Ischemic Conditions: In models of hind limb ischemia, where blood flow is obstructed, BPC-157 has been observed to stimulate NO release and promote the formation of collateral blood vessels (arteriogenesis) to bypass the blockage.
- Interaction with NOS Blockers: Preclinical studies have demonstrated that BPC-157 can counteract the effects of L-NAME (a specific inhibitor of nitric oxide synthase), suggesting it possesses a robust capacity to maintain NO signaling even under chemical inhibition.
Preclinical Research Models: Where Angiogenesis Matters
The theoretical mechanisms of VEGFR2 and NO signaling have been tested in various animal models to observe macroscopic outcomes. Research has focused on tissues where vascularization is the primary hurdle to healing.
1. Tendon and Ligament Repair
Tendon and ligaments are notoriously slow to heal due to their low metabolic rate and poor blood supply. Research investigating the "bone-tendon junction" in rat models has reported that BPC-157 administration is associated with increased capillary density at the injury site.
2. Skeletal Muscle and Ischemia
In studies involving crushed muscle tissue or surgically induced ischemia, researchers measure "blood flow recovery" using laser Doppler imaging. Data indicates that subjects treated with BPC-157 often exhibit faster restoration of perfusion compared to controls.
3. Granulation Tissue Formation
Granulation tissue is the new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process. In models of severe skin damage (such as alkali burns), BPC-157 has been linked to accelerated granulation tissue formation via the upregulation of growth factors like EGR-1 and VEGF.
Vascular Remodeling and Stability
Angiogenesis is not merely about sprouting new vessels; those vessels must mature and stabilize to function correctly. This process is known as vascular remodeling.
Research suggests that BPC-157 may influence the stability of vascular structures. In models of vasculitis or vessel damage, the peptide has been investigated for its ability to preserve endothelial integrity. By potentially mitigating the "leakiness" of newly formed vessels, BPC-157 may support the development of a functional, rather than just abundant, vascular network.
Summary of Scientific Consensus
The body of research surrounding BPC-157 paints a picture of a peptide with significant potential to influence vascular biology. The consensus across multiple preclinical studies is that BPC-157:
- Activates the VEGFR2-Akt-eNOS pathway to drive endothelial cell proliferation.
- Modulates nitric oxide production to support vasodilation and vessel survival.
- Accelerates blood flow recovery in ischemic, damaged, or hypovascular tissues.
Conclusion
For researchers in biotechnology and tissue engineering, BPC-157 represents a unique compound of interest. Its ability to stimulate angiogenesis through established molecular pathways—specifically the VEGFR2 and NO systems—positions it as a candidate for further study in the context of wound healing, ischemic recovery, and soft tissue repair.